how to: oxygen devices
Dr. Martha Gallegos
Introduction:
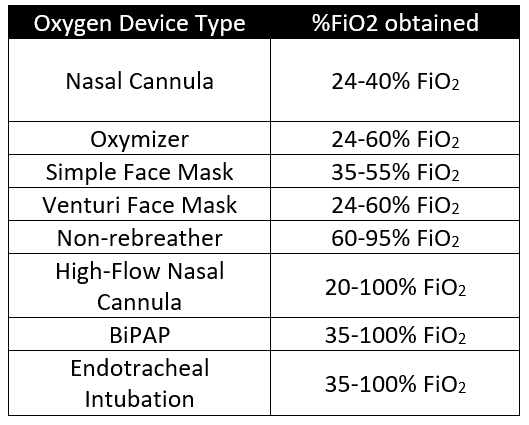
When considering oxygen delivery devices, it is essential to consider the needs of the patient and any contraindications to those modalities. While there are many styles of oxygen delivery modalities, they function differently. For example, some oxygen modalities can provide low flow oxygen amounts due to their dependence on patients on minute ventilation, such as the nasal cannula and the simple face mask. Other oxygen modalities provide fixed amounts of oxygen regardless of the patient’s minute ventilation, thus making them easily titratable. These are the Venturi face mask and the high flow nasal cannula. This blog will walk you through the various oxygen modalities available to provide supplemental oxygen for the patients.
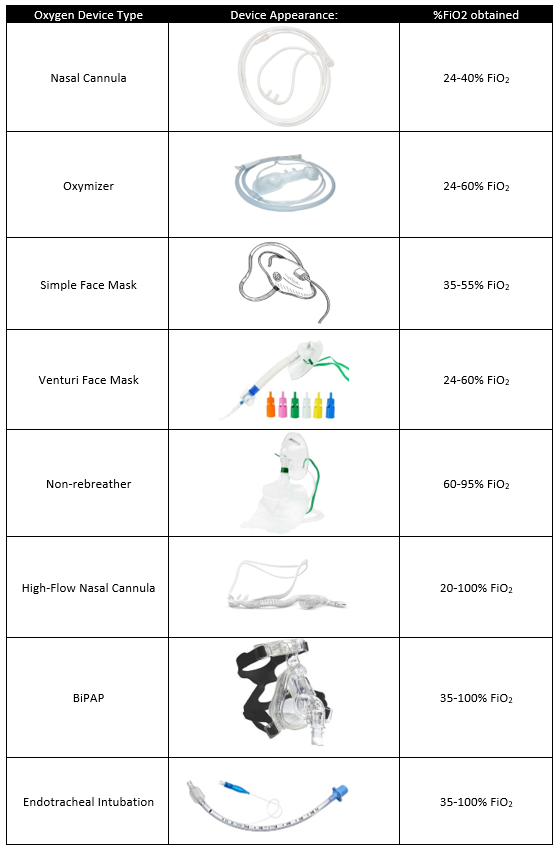
The Oxygen Delivery Devices
Nasal cannula – can provide 1-6L/min (24-40% FiO2), the most recognized form of oxygen delivery used. However, it is important to remember that patient’s total amount of oxygen delivery is also dependent on the patient’s ventilatory demands, leading to an even smaller quantity of oxygen delivery flow to patients.
Oxygen Reservoir Nasal Cannula – can provide up to 15L/min of oxygen (24-60% FiO2) close in appearance to the nasal cannula but with the addition of bilateral oxygen reservoir in the formation of a mustache, also known as the Oxymizer. The reservoir allows for an increased quantity of oxygen successfully delivered to a patient.
Simple Face Mask – can provide 5-10L (35-55% FiO2). The face mask covers both nares and the mouth while providing a small reservoir within the face mask tent. The simple face mask also has bilateral exhalation ports that allow the entrance of room air. Like the nasal cannula, the exact amount of oxygen delivery can vary depending on the patient’s ventilatory demands.
Venturi Face Mask – can provide 2-15L (24-60% FiO2). Unlike the simple face mask, this mask provides a fixed amount of oxygen delivery regardless of the patient’s current minute ventilation also known as the air-entrapment mask. Therefore, it is ideal for patients requiring larger amounts of oxygen but allows one to titrate the quantity of oxygen delivered to maintain target spO2.
Non-rebreather – can provide 10-15L/min (60-95% FiO2) using an oxygen reservoir that patient breathes from with a one-way valve present that prevents the patient from breathing in expired air. Non-rebreathers must be used at a rate higher than a patient’s minute ventilation and should not be used to administer oxygen below 10L.
High-Flow Nasal Cannula – can provide 40-60L/min (20-100% FiO2). The high-flow nasal cannula can provide a fixed rate of oxygen and provide a higher quantity of oxygen flow and FiO2 needed in patients with severe hypoxemia while avoiding more invasive measures of oxygenation. Contraindications to this device include recent nasal passage surgery, epistaxis, and skull trauma.
BiPAP – can provide up 35-100% FiO2. Unlike other oxygen modalities, the BiPAP functions by providing bi-level positive airway pressure dependent on exhalation and inhalation. Contraindications to this device include uncontrolled emesis, facial trauma, epistaxis, and altered mental status. This will be discussed in further detail in a separate blog.
Endotracheal Intubation – can provide 35-100% FiO2. Endotracheal intubation is the most invasive form of oxygen modalities, and most effective form of providing oxygen. The decision of when to intubate is complex and should consider patient’s overall goals of care as well as goal for oxygenation. This will also be discussed in further detail in a separate blog post
Conclusion:
When electing an oxygen delivery device, always consider how much oxygen a patient needs or what the target is, can the patient tolerate the delivery device I plan to use, and are there any contraindications to using the device. Oxygen delivery devices such as non-rebreather and venturi masks can help stabilize a patient before selecting the most appropriate device to treat the patient’s hypoxemia.
Martha Gallegos, M.D.
Dr. Martha Gallegos is a second-year members of the University of Louisville Internal Medicine Residency Program.
Medical school: University of New Mexico
Residency: University of Louisville Hospital
Reference:
Batool S, Garg R. Appropriate Use of Oxygen Delivery Devices. The Open Anesthesia Journal. 2017;11(1). doi:10.2174/1874321801711010035
Hardavella, Georgia & Karampinis, Ioannis & Frille, Armin & Sreter, Katherina & Rousalova, Ilona. (2019). Oxygen devices and delivery systems. Breathe. 15. e108-e116. 10.1183/20734735.0204-2019.
Marino P. The ICU Book. 4th ed. Wolters Kluwer Health/Lippincott Williams & Wilkin
Segmueller C. Oxygen delivery devices. Anesthesia Airway Management (AAM). Published 2018. Accessed November 24, 2021. https://aam.ucsf.edu/oxygen-delivery-devices