Don’t Pop the Clot
Permissive Hypotension for Uncontrolled GI bleeds: Should we be doing it?
Dr. Dylan Gerlach
Gastrointestinal bleeding is a commonly encountered problem in the inpatient setting. Current treatment guidelines recommend maintaining a mean arterial pressure (MAP) greater than 65 mmHg, similar to other medical patients. An abundance of trauma surgery literature has provided guidance for uncompressible bleeding sites due to trauma by appropriately adjusting MAP goals based on the clinical picture and allowing hypotension in various settings, termed permissive hypotension. So, should this be carried over to the GI bleed setting since it is also uncompressible and has it been looked at before? That’s what we are here to find out.
Body’s response to hemorrhage
The body has normal intrinsic coagulation pathways that are activated to achieve hemostasis as rapidly as possible. Immediately after vascular injury, arterial vasospasm occurs to decrease blood loss through the site of injury. Primary hemostasis results in the formation of a platelet plug, which is fragile until stabilized through activation of the clotting cascade with resulting formation of a fibrin clot.
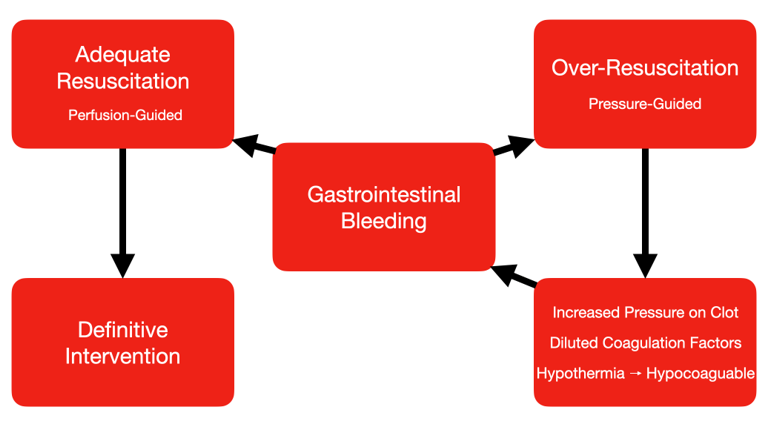
Problems of early aggressive resuscitation
There is potential that the increase in hydrostatic pressure, can cause a fragile platelet plug or newly-formed fibrin clot to break off, thus limiting autoregulation of hemorrhage
When Intravenous fluids or blood is transfused, there is a dilution of the clotting factors which makes the patient hypocoaguable and more likely to bleed.
Additionally, unless the fluid or blood is run through a warmer, it makes the patient more hypothermic which also makes the makes hypocoagulable.
This triad of increased hydrostatic pressure, dilutional hypocoagulability, and hypothermia leads to a spiral of more bleeding and more resuscitation.
Is permissive hypotension the answer?
Permissive hypotension is a term that defines the approach for allowing blood pressure to be maintained at lower target goals and is guided by the clinical picture including vital signs, mental status and other indicators of sufficient tissue perfusion.
Studies utilizing permissive hypotension typically maintain either a MAP of 50 mmHg or systolic blood pressures between 80 and 90 mmHg
What are the goals of utilizing a permissive hypotension approach?
Avoid over-resuscitation with fluids
Provide adequate support only when perfusion needs can no longer be met on their own
Provide individualized patient-centered care, avoid generalized treatment approaches that may not be patient-specific
Avoid exacerbating hemorrhage by disrupting normal intrinsic coagulation (“pop the clot”)
Some potential benefits?
Many cirrhotic patients, who are much more likely to have GI bleeding, typically have altered hemodynamics with splanchnic and peripheral vasodilation leading to a decreased peripheral vascular resistance that is all the result of prolonged portal hypertension.
In longstanding cirrhotics, it may be difficult to achieve generalized MAP parameters, thus providing potential benefit for a permissive hypotension approach
While no RCT currently exists examining a permissive hypotension approach specifically targeting patients with GI bleeding, there may be no difference in mortality as compared with early and aggressive fluid resuscitation (if we extrapolate data from trauma-specific cohorts)
So what’s the evidence?
Several studies have shown that there is no difference in mortality in trauma patients who are treated using permissive hypotensive goals than those treated with standard-of-care MAP goals greater than 65 mmHg. Currently, there were no available studies focused on permissive hypotension in patients with gastrointestinal bleeding. A 2014 meta-analysis looked at the timing and volume of fluids for bleeding. It looked at 6 trials with a combined 2128 patients. They did not find a difference in mortality in trauma patients who were treated with early and aggressive fluid resuscitation. A systematic review and meta-analysis specifically looking at permissive hypotension with BP targets 50-70 mmHg or MAP of 50 mmHg or more. 4 of the 5 trials suggested a mortality benefit with permissive hypotension. Three of them were not powered sufficiently and they had concerns with lack of blinding and reporting methods. The pooled odds ratio was 0.70 (95% confidence interval, 0.53–0.92) showing a survival benefit for patients treated with permissive hypotension.
While there have not been any studies looking at permissive hypotension in upper GI bleeds, transfusion strategies for acute upper GI bleed was published in 2013 and showed at there was no difference between transfusing to 7g/dL vs 9g/dL. There was a subset analysis of cirrhotic patients which showed a mortality benefit with transfusing to 7g/dL. A case could be made that this mortality benefit is from the prevention of the resuscitation provoked bleeding triad. The lower transfusion threshold led to less hypocoagulation, less hypothermia, and less hydrostatic pressure.
Of note, a recently published interventional algorithm regarding the management of GI bleeds addresses the need for vasopressor medications after initial appropriate fluid and blood resuscitation is achieved that allows for permissive hypotension until definitive therapy can be performed. While no outcomes are observed based on utilizing a permissive hypotensive approach compared to those that seek to achieve the standard MAP goal of 65, the recognition that permissive hypotension is an appropriate target in this particular setting is worth acknowledging.
Caveats
Patients with TBI or other head injury/stroke may require higher BP targets and thus permissive hypotension approach should not apply
Permissive hypotension approach does not negate the importance of adequate initial resuscitation if the patient is in shock and showing signs of poor perfusion
Our Take on the Matter
While the data behind utilizing a permissive hypotension approach, specifically related to patients with GI bleeding, is not yet available, there is potential that a patient-centered approach utilizing clinical exam other hemodynamic parameters may be fruitful in changing the way we manage patients in these critical settings
If a patient has a massive GI bleed and is in shock, don’t wait for the labs – transfuse immediately, transfuse appropriately
After initial transfusion, re-examine the patient – check the signs of tissue perfusion, assess mental status. Is the patient being adequately perfused after transfusion? Assess blood pressure and heart rate and their respective trends. Is the patient still hypotensive? If the patient has signs of adequate perfusion, consider utilizing permissive hypotension approach while awaiting therapeutic intervention.
After the appropriate therapy has been addressed, reassess vital signs and determine if further fluid resuscitation is appropriate in order to target a more standardized MAP goal of 65 mmHg
Dylan Gerlach, D.O.
University of Louisville | UL · Department of Medicine | Doctor of Osteopathic Medicine
Dr. Dylan Gerlach is a PGY 3 at the University of Louisville Internal Medicine Residency Program. Dr. Gerlach completed Medical School at the University of Pikeville in Pikeville, Kentucky.
References:
Palta S, Saroa R, Palta A. Overview of the coagulation system. Indian J Anaesth. 2014;58(5):515-523. doi:10.4103/0019-5049.144643
Kwan I, Bunn F, Chinnock P, Roberts I. Timing and volume of fluid administration for patients with bleeding. Cochrane Library 2014; 3: CD002245.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL: Survivign Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 2008, 34: 783-785. 10.1007/s00134-008-1040-9
Kwan I, Bunn F, Chinnock P, Roberts I. Timing and volume of fluid administration for patients with bleeding. Cochrane Database Syst Rev. 2014 Mar 5;2014(3):CD002245. doi: 10.1002/14651858.CD002245.pub2. PMID: 24599652; PMCID: PMC7133544
Tran, Alexandre MD; Yates, Jeffrey MD; Lau, Aaron MD; Lampron, Jacinthe MD; Matar, Maher MD Permissive hypotension versus conventional resuscitation strategies in adult trauma patients with hemorrhagic shock: A systematic review and meta-analysis of randomized controlled trials, Journal of Trauma and Acute Care Surgery: May 2018 - Volume 84 - Issue 5 - p 802-808 doi: 10.1097/TA.0000000000001816
Rodrigues A, Carrilho A, Almeida N, et al. Interventional Algorithm in Gastrointestinal Bleeding-An Expert Consensus Multimodal Approach Based on a Multidisciplinary Team. Clin Appl Thromb Hemost. 2020;26:1076029620931943. doi:10.1177/1076029620931943