Drowning and Resuscitation: It’s ABC not CAB
Dr. Elizabeth Lehto
Samantha is a 3-year-old female who presents after being found face down in the family pool. She was last seen 20-minutes prior to being found in the pool. On arrival to the emergency department, she has a weak cry and is only intermittently responsive to tactile stimuli. She was intubated for airway protection and an orogastric tube was placed with return of a large volume of clear water. She was admitted to the pediatric intensive care unit for further management.
Every year in the United States there are an estimated 3,960 fatal unintentional drownings and 8,080 nonfatal drownings.¹
Multiple definitions of drowning have been used in the medical literature, which can create confusion. To alleviate this confusion, the recommended definition of drowning is: a process resulting in primary respiratory impairment from submersion/immersion in a liquid medium. Accordingly, the term “drowning” should be used regardless of outcome, and modifiers including near, wet, dry, secondary, active, passive, and silent should be abandoned.²
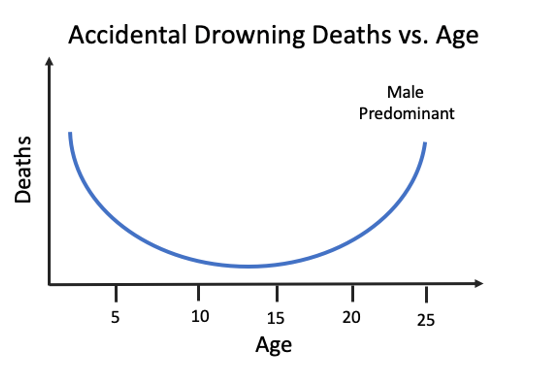
Drowning is a common cause of accidental death in the United States and has a bimodal distribution. The first peak occurs in children less than five who are inadequately supervised around water, the second peak is among males between 15 and 25 years old and tend to occur at rivers, lakes, and beaches.³
Prehospital Care:
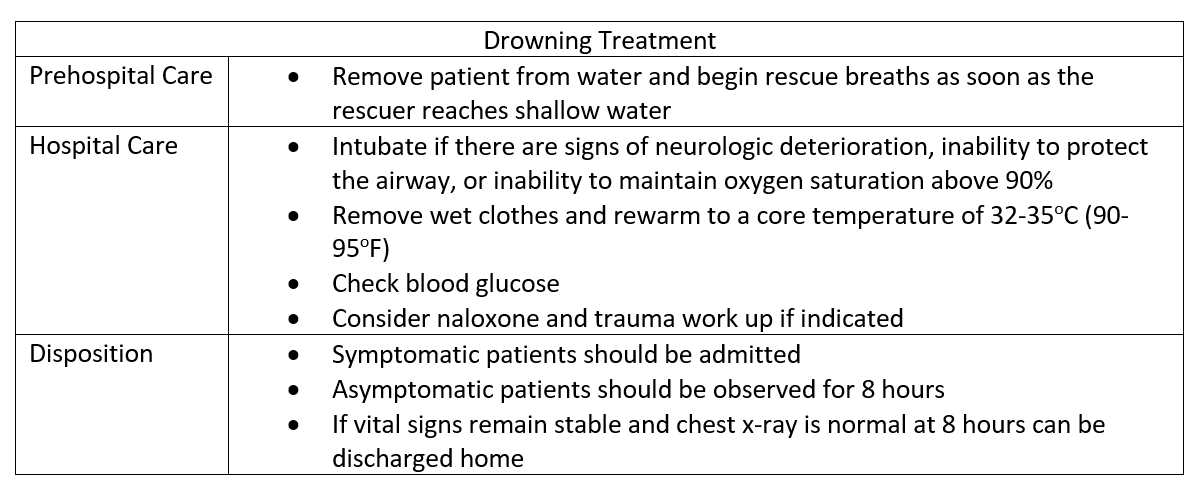
In the severely affected drowning victim, the critical moments in care generally occur prior to arrival of medical professionals. The most important step is prompt removal from the water and immediate determination for need of bystander cardiopulmonary resuscitation (CPR).⁴ Ventilation is the most important treatment, and rescue breaths should begin as soon as the rescuer reaches shallow water or a stable surface. If the patient does not respond to the delivery of two rescue breaths that make the chest rise, the rescuer should immediately begin chest compressions.
Note, in drowning victims the order of resuscitation efforts is airway, breathing compressions (ABC). This is different than the typical adult cardiac arrest patients that emphasizes immediate uninterrupted chest compressions followed by airway and breathing (CAB). This is because cardiac arrythmias seen in drowning are almost exclusively secondary to hypoxia.⁵
Hospital Care:
Symptomatic patients should be intubated if there are signs of neurologic deterioration, inability to protect the airway, or inability to maintain oxygen saturation above 90% despite use of a high-flow oxygen-delivery system or noninvasive ventilation. If tracheal intubation is performed, an orogastric tube should be placed to relive gastric distention. Symptomatic patients who do not require immediate intubation should be provided supplemental oxygen to maintain oxygen saturation above 94%.⁶
Bedside glucose should be measured soon upon arrival to the emergency department. Naloxone should be considered in cases when opioid intoxication may be a factor. Trauma evaluation should be performed and imaging studies obtained as indicated. Cervical spine precautions should be taken if there is a concerning history, such as a dive into shallow water, or signs of injury.⁵
Wet clothing should be removed and rewarming initiated in hypothermic patients. Rewarming methods include external (both passive and active including warm blankets, heating pads, and radiant heat) as well as active internal rewarming (including warmed humidified oxygen and heated irrigation of peritoneal and pleural cavities).⁵
In hypothermic patients, resuscitative efforts should be continued until core temperature reaches 32-35oC (90-95oF).⁷ Hypothermic patients may have complete recovery despite prolonged resuscitation, whereas normothermic patients are likely to have poor outcomes if return of spontaneous circulation does not occur within 30 minutes of initiation of advanced life support.⁸,⁹
Disposition:
Symptomatic patients:
Symptomatic patients should be admitted and monitored until symptoms resolve. Electrocardiography, serum electrolytes, creatine, and assays for alcohol and illicit drugs are recommended for adolescent and adult patients.⁵
Asymptomatic patients:
Asymptomatic patients should be observed for 8 hours and admitted if any deterioration occurs. A chest radiograph should be obtained on arrival and again at 8 hours in asymptomatic patients. If radiography and vital signs are normal and no clinical deuteriation occurs during the 8 hour observation period, the patient may be discharged.⁵
Prevention:
The most important intervention to improve outcomes form drowning is prevention.
Supervision:
Children should be supervised anytime they are near water. When several adults are present, one should be designated the “Water Watcher.” The water watcher agrees to watch children for a set amount of time without distraction. Having the water watcher wear a card or bracelet can be helpful to clearly identify who is filling that role. It is important to remember that supervision is not foolproof. A child can enter the water during even the briefest lapse in attention. Most childhood drownings are silent, so listening for child splashing or struggling is not a reliable method of supervision.
Life Saving Skills:
Everyone should know the basics of swimming and CPR. Many children can begin swim lessons as early as age one, and by age four most children are ready for swim lessons. Several CPR course options are available including from the American Heart Association and the American Red Cross.
Barriers to Entry:
All swimming pools should have a four-sided isolation fence with self-latching gates. Pool fences should completely separate the house and any play areas from the pool. Fencing should be at least 4-feet high and have no openings under it or between slats that are more than 4 inches wide. Such fencing can reduce the incidence of drowning by 50-80%.⁴ Keeping toys out of the pool area when the pool is not in use can help prevent children from trying to get through the fence during non-swim time.
Life Jackets:
Children should wear life jackets around natural bodies of water such as lakes or ocean, even if they know how to swim. Adults should wear life jackets while boating or enjoying other recreational water sports.
Avoid Alcohol:
Use of alcohol and illicit substances greatly increase drowning risk and should be avoided when participating in or supervising water activities.
Prevention Resources:
Summary:
The term drowning should be used regardless of outcome, modifiers should be avoided to prevent confusion. The most important intervention to improve outcomes from drowning is prevention. Preventative efforts include adequate supervision, pool fencing, and water safety education. Once drowning has occurred, rapid recue and effective bystander resuscitation is key to reducing morbidity and mortality, therefore efforts should focus on training the public on how to preform efficient cardiopulmonary resuscitation.⁴ Symptomatic patients should be admitted, patients who are asymptomatic after 8 hours of observation can be discharged.
Case Follow-up:
Returning to our patient, Samantha was able to be extubated while the pediatric intensive care unit and is expected to make a full recovery.
Elizabeth Lehto, D.O.
University of Louisville | UL · Department of Pediatrics | Doctor of Pediatric Emergency Medicine
Dr. Elizabeth Lehto is a Pediatric Emergency Medicine Attending at Norton Womens and Children’s Hospital. Dr. Lehto attended Midwestern University Arizona College of Osteopathic Medicine and completed her residency and fellowship at the University of Louisville.
References
CDC. Drowning Facts. 2021; https://www.cdc.gov/drowning/facts/index.html. Accessed July 1, 2021.
Schmidt AC, Sempsrott JR, Szpilman D, et al. The use of non-uniform drowning terminology: a follow-up study. Scand J Trauma Resusc Emerg Med. 2017;25(1):72.
DeNicola LK, Falk JL, Swanson ME, Gayle MO, Kissoon N. Submersion injuries in children and adults. Crit Care Clin. 1997;13(3):477-502.
Meyer RJ, Theodorou AA, Berg RA. Childhood drowning. Pediatr Rev. 2006;27(5):163-168; quiz 169.
Chandy D, Weinhouse GL. Drowning (submersion injuries). 2020; https://www.uptodate.com/contents/drowning-submersion-injuries?search=drowning&topicRef=177&source=see_link.
Layon AJ, Modell JH. Drowning: Update 2009. Anesthesiology. 2009;110(6):1390-1401.
Jolly BT, Ghezzi KT. Accidental hypothermia. Emerg Med Clin North Am. 1992;10(2):311-327.
Giesbrecht GG. Cold stress, near drowning and accidental hypothermia: a review. Aviat Space Environ Med. 2000;71(7):733-752.
Kieboom JK, Verkade HJ, Burgerhof JG, et al. Outcome after resuscitation beyond 30 minutes in drowned children with cardiac arrest and hypothermia: Dutch nationwide retrospective cohort study. Bmj. 2015;350:h418.