Continuing to Survive Sepsis with Some Changes
Dr. Will Linville
Walk into any ICU on any given day and there will be a patient who is suffering from sepsis. Arguably, the most common diagnosis that the ICU physician encounters and a diagnosis that requires rapid recognition and treatment. ICU physicians have been trained to follow surviving sepsis guidelines which have gone through updates over the years since their first launch in 2002. We now have the 2021 updates, and I would like to go over some of those most important updates with you. Hopefully this will be informative and save you from having to read a 60 page document.
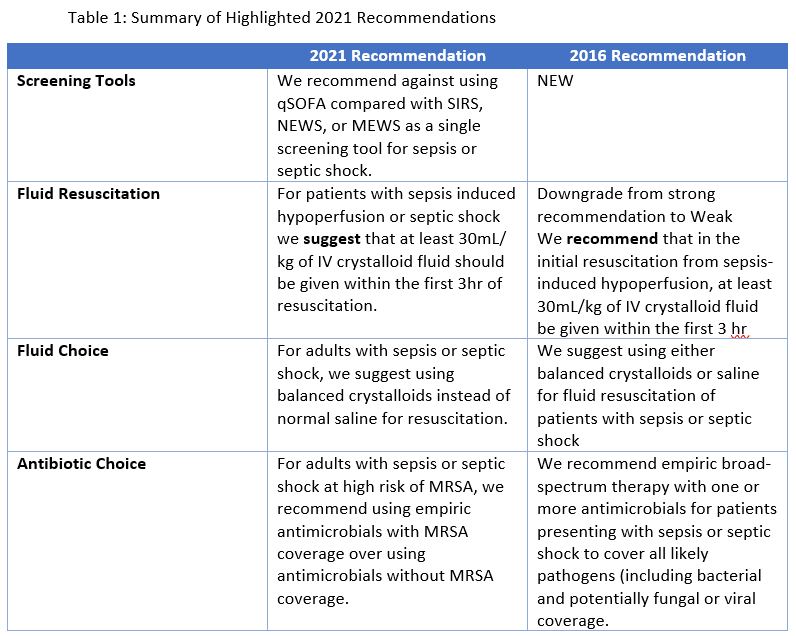
A key update for the 2021 sepsis cycle was a recommendation to no longer use qSOFA as a screening tool. Traditionally, this has been taught to med students and medicine residents everywhere. The qSOFA is a simple and quick assessment using three parameters: a Glasgow Coma Score < 15, a respiratory rate ≥ 22 breaths/min and a systolic blood pressure ≤ 100mm Hg. A positive score was considered when at least two parameters were present. The research behind qSOFA that initially prompted the recommendation to use it as a screening tool only showed that it predicted poor outcome in patients with known or suspected infection. There has been no data analysis showing usefulness as a screening tool. The document goes on to mention that only 24% of infected patients in the original study had a positive qSOFA but those patients accounted for 70% of bad outcomes. With this acknowledgement, their new recommendation is to utilize SIRS, NEWS, or MEWS for screening of sepsis. They specifically mention studies looking at SIRS and qSOFA which showed that while qSOFA is more specific than SIRS, it is less sensitive than having 2 of the 4 SIRS criteria. Remember from Biostats (it never goes away), sensitivity reflects a test’s accuracy in identifying disease in people who truly have the disease. For these reasons, Surviving Sepsis no longer recommends qSOFA as a single screening tool but rather a tool for outcome prediction once you have diagnosed sepsis.
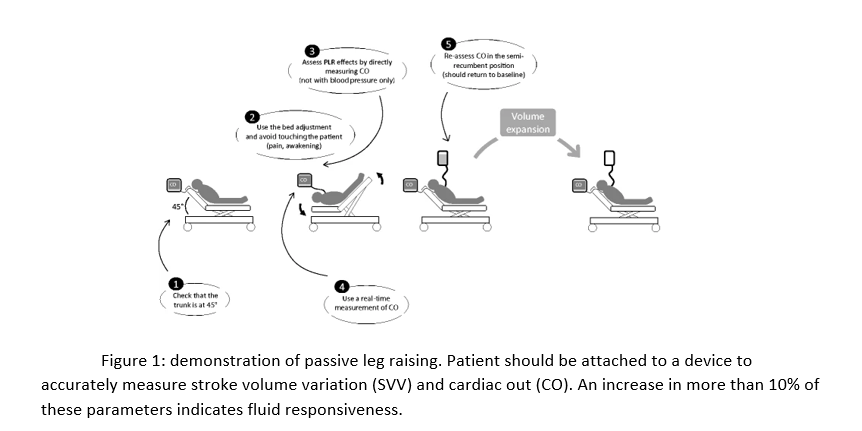
Another major change in recommendations that came down the pipeline concerned fluid resuscitation in sepsis. For some time, the knee jerk reaction in sepsis has been intravenous fluids at 30mL/kg, AKA the “Sepsis Bolus”, but then providers go on to give the patients more fluid boluses or a “maintenance” rate. In 2021, this sepsis bolus has been downgraded to a weak recommendation. The 2016 recommendations were based on observational data and no prospective studies have shown an ideal amount of initial resuscitation. They suggest the initial bolus but then move forward by suggesting active measures to assess whether the patient needs further resuscitation. The continued resuscitation must be balanced with the risk of increased fluid overload. The 2021 campaign mentions that dynamic measurements should be used to assess the need for further resuscitation. These measures are passive leg raising (figure 1) combined with cardiac output (CO) measurement, fluid challenges against stroke volume (SV), systolic pressure or pulse pressure, and increases of SV in response to changes in intrathoracic pressure. CVP is mentioned as being a poor indicator of volume and is not recommended.
Pertaining to fluids, there was also a change concerning the choice of fluid for resuscitation in sepsis. In past guidelines, it was recommended that a provider use crystalloid as compared to colloids. However, in the newest guidelines, it is taken one step further and there is a recommendation for which crystalloid should be used. The new recommendation is considered weak but states that they suggest that balanced crystalloids should be used instead of normal saline. I will note that it has been seen in practice that ICU physicians are moving away from normal saline in sepsis, but this is the first time that Surviving Sepsis is officially making a recommendation about choice of crystalloid. This data is developed out of examining the data from the SMART trial. This trial was published in 2018 and it was a single center trial that examined 15,802 patients. The recommendation is due to a subgroup of patients admitted with sepsis in all participating ICUs which showed a lower 30-day mortality in the balanced crystalloids group. There was also a secondary analysis of septic patients admitted to the Medical ICU in which balanced crystalloids were associated with an improved 30-day mortality, and higher vasopressor and RRT-free days.
The final recommendation that I will discuss pertains to antibiotic choice in sepsis. Think about a patient being admitted for septic shock and the provider is ordering antibiotics. Which antibiotics are they ordering? I am willing to bet that you thought “Vanc and Zosyn”. This final recommendation pertains to that choice of Vancomycin. The past 2016 guidelines officially stated, “We recommend empiric broad-spectrum therapy with one or more antimicrobials for patients presenting with sepsis or septic shock to cover all likely pathogens (including bacterial and potentially fungal or viral coverage”. This was extremely vague and thus you have the birth of Vanc and Zosyn or Vosyn, as I call it. The new recommendation specifically pertaining to MRSA coverage states that risk of MRSA should be assessed in each patient. If a patient is at low risk of MRSA coverage, then they recommend against using antimicrobials with MRSA coverage. They cite some data to support not blindly placing Vancomycin on patients. Firstly, MRSA accounts for approximately 5% of culture positive infections among critically ill patients and there is evidence that it could be decreasing. There are studies in patients with undifferentiated pneumonia or sepsis who had MRSA coverage that showed higher mortality. Interestingly, this increase in mortality was most evident in patients who were shown to not have MRSA infections. While it could be harmful to miss a MRSA infection, it could be just as harmful to place MRSA coverage on someone who does not need it. Therefore, they recommend assessing MRSA risk factors. Risk factors for MRSA include prior history of MRSA infection or colonization, recent IV antibiotics, history of recurrent skin infections or chronic wounds, presence of invasive devices, hemodialysis, and recent hospital admission.
While the document covers many more recommendations, these are the ones that seem newest and most relevant for the ICU physician. Sepsis is an ever-growing diagnosis and treatments will change constantly. I invite providers to continue to follow the evidence to give their patients the best care.
Will Linville, D.O.
Medical school: Lake Erie College of Osteopathic Medicine, Erie, PA
Residency: University of Louisville Hospital
About William: I grew up in a small town in Ohio, completed med school in Pennsylvania, and came to Kentucky for residency and fellowship. If I'm not working then you can find me spending time with my wife, dog, or video games. I love ICU and look forward to teaching the residents during my time at UofL.
Hobbies: Video games, lifting, hiking, and cars/motorcycles
Favorite Restaurant in Louisville: Game - you have to try the kangaroo burger!
Research interests: COPD, Sepsis
References:
Sepsis 2021